ihumaxn
20 January 2025
No Comments
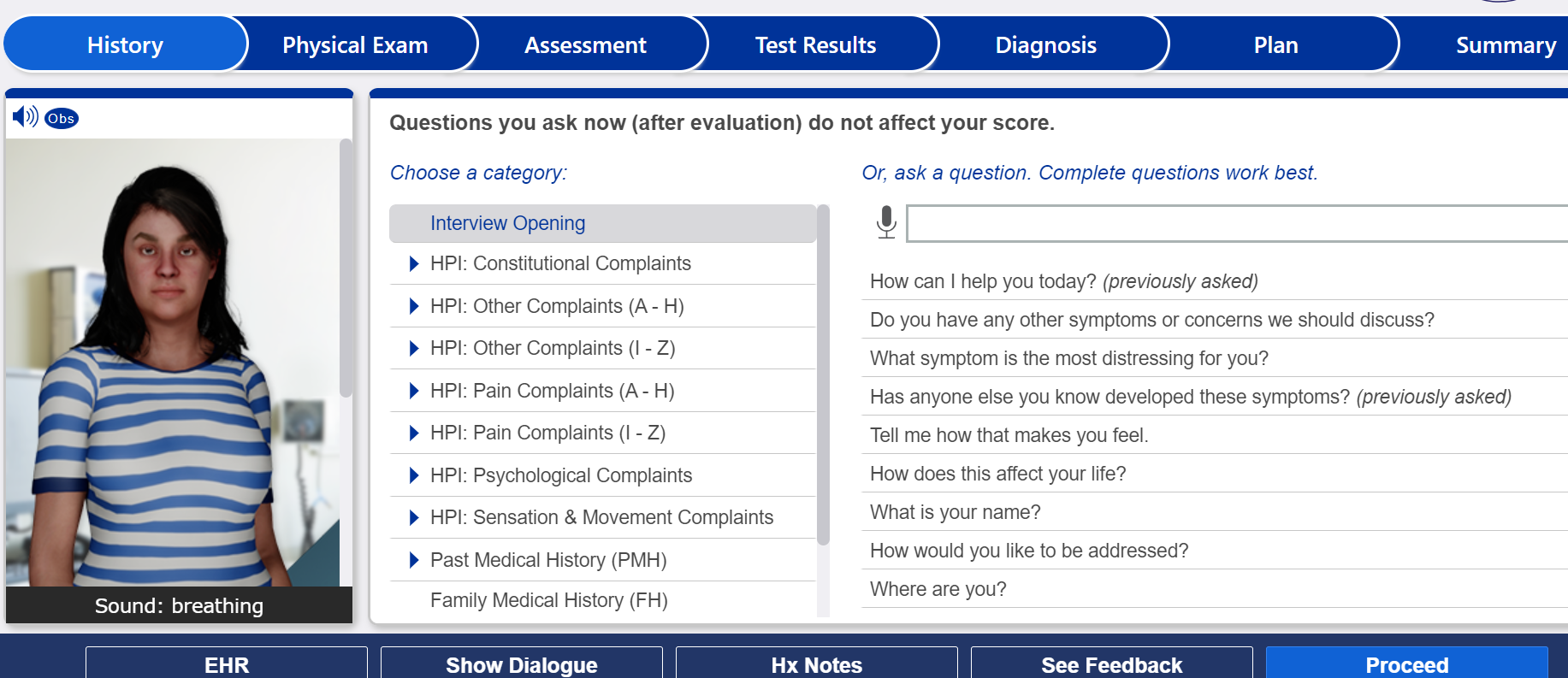
Passing iHuman Cases
EHR Documentation Tips for i-Human
I wanted to address some of the issues I am finding with documentation of the iHuman assignments, and provide some general tips to assist you with provider documentation when completing these assignments:
Remember all documentation must be completed in the EHR
OLDCARTS is a mnemonic used to assist providers with obtaining the history of present illness (HPI) of the patient. You should use this method to assist you when completing the iHuman assignments and obtaining the history.
O-onset (when did the patient’s condition begin)
L-location (where the patient feels the sensation, for example pain)
D-duration (how long the patient has had the condition)
C-character (what does the symptoms feel like)
A-aggravating factors (what makes the symptoms worse)
R-relieving factors (what makes the symptoms better)
R-radiation (whether the symptoms spreads to other parts of the body)
T-timing (when the symptoms occur)
S-Severity (how bad are the symptoms)
Example only You are asked to write the HPI please start with statement like this:
24-year-old female presented to the clinic with chief complaint of (whatever it is). Then document the HPI including the 7 different components that I have listed above (using OLDCARTS). This should ensure that you include all 7 components.
Subjective info includes the CC, HPI, PMH, meds, allergies, FH, SH and ROS.
It is important that you understand the difference between subjective and objective information, and where each is documented.
***Under general category for subjective information please do not write alert and oriented as this is objective information that goes in the PE. Do not place vital signs in the subjective area as it should be with the PE unless you are documenting something like the patient reports a temp of 102. ***
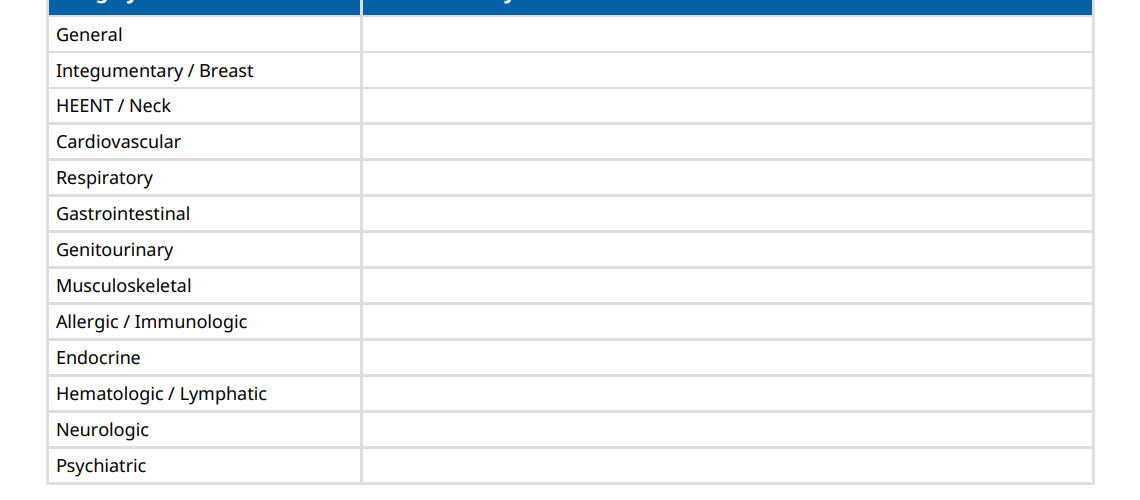
Complete all the systems in the ROS with subjective information only. This is what the patient tells you or a history of something. For example, if a patient has hx of diabetes, then under Endocrine system- you could document pt. has hx of diabetes, denies increased thirst and frequent urination.
You should not document normal or none but list the specific symptoms the patient admits to or denies.
Objective information is the PE, diagnostic tests, plan
PE should be in detail. Objective data is measurable; therefore, providers should NEVER use the words normal, abnormal or WNL.
Providers should use the correct medical terminology and document what is heard, seen or felt when completing a PE on a patient.
What do the heart, lungs, abdomen sound like for example. I expect to see detail in the assessment findings and not just general info such as regular rate and rhythm.
Please be specific if you are palpating the sinus area then identify the sinuses area you are referring to (frontal, maxillary or where), and same with lymph nodes.
If you are documenting edema, where is it located and how is it measured? If you document capillary refill, then it should be less than a certain number of seconds.
You are asked to write a problem statement; please review the criteria. It tells you there must be both subjective and objective information in that statement. If it is not there you will lose points per grading rubric.
You are asked to develop 3 differential diagnoses which you should clearly identify in the plan. What diagnostic tests would you use to assist in diagnosing the patient and why?
The management plan should be detailed and include references per the assignment grading rubric. You are instructed to provide rationales for your interventions in the management plan; therefore, you should have references. You are to write medication as complete RX, and if the patient requires consult/referrals and a follow up plan. The f/u plan should include detailed. For instance, who should the patient follow up with and when. What should the patient do if the symptoms do not resolve and become emergent?
In detail, what is the patient education that you will provide for the patient and why, with references included.
Therefore, if clinical practice guidelines are omitted, references are not used, and the questions of the assignment are not answered you will lose points as noted in the grading rubric. The grading rubric has this all listed. Finally, if a question is asked; for example, what labs does the patient need, and you do not think the patient needs any then you should state this and explain why. If you leave it blank, then guess what you will lose points because you did not address the question.
Finally, please remember to use scholarly references. Therefore, DO NOT USE MAYO OR CLEVELAND CLINIC as they are NOT scholarly, and you will lose because of this.