iHuman Step by Step
History, Physical Examination, Diagnosis INSTRUCTIONS
Typically, iHuman case studies are graded in the following manner:
- History 40%
- Physical exam 40%
- Plan 20% (faculty scored)
Remember, At iHumanHelp.com, we offer expert support for completing your I-Human assignments, case studies, quizzes, and exams. Our services guarantee an A on your I-Human cases with no payment required until you’re fully satisfied. Chat with Us
HISTORY:
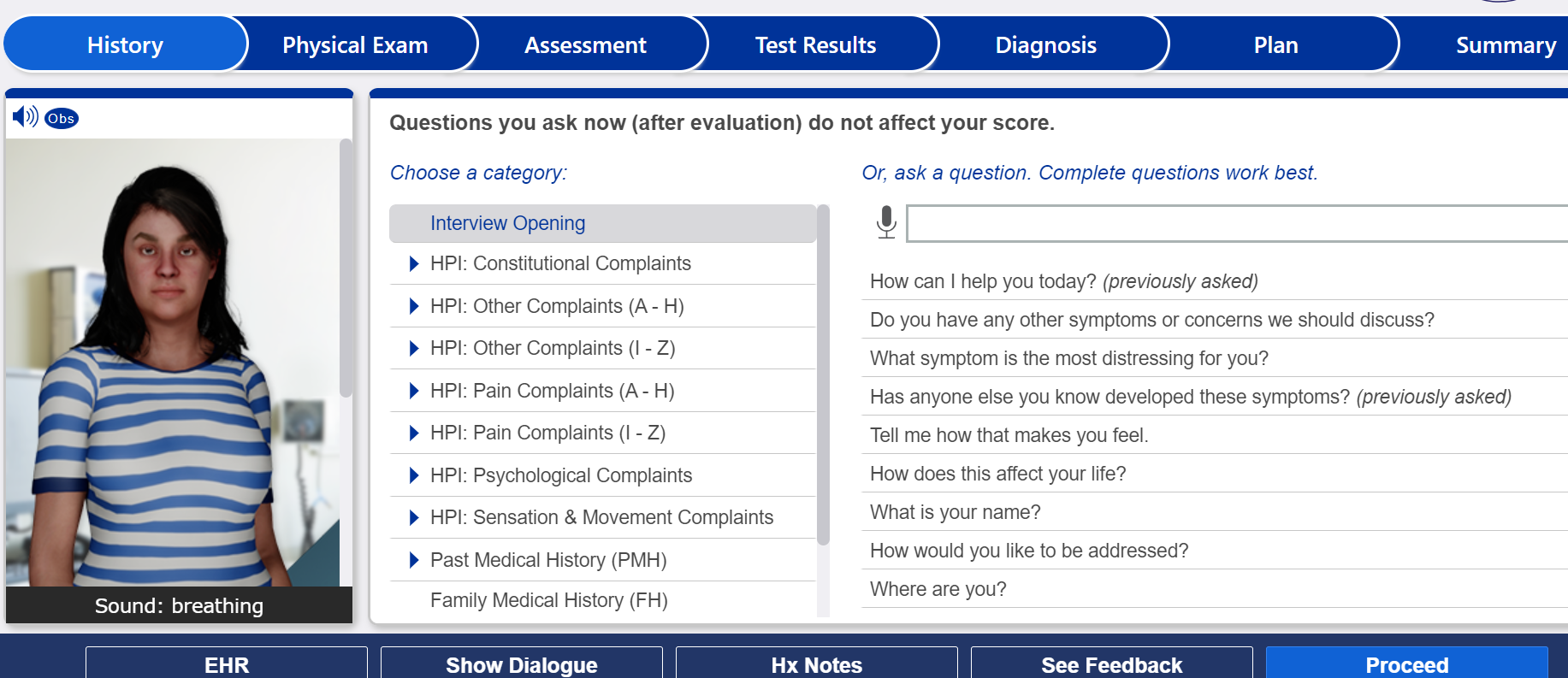
- To ask questions, you may type into the search box and select your desired question, or you may use the pre-populated question bank in the middle of the screen to search by category and select your desired question.
- “Good Question!” means you have asked a required question.
- Notate your Key Findings in the “Key Findings” section, and document your History in the EHR.
HISTORY QUESTION LIMIT:
- You can ask a limit of 90 questions.
HISTORY HINTS:
- You may access the “Hx Hints” button 5 times.
- Click on the button for hints on the remaining required questions to ask your patient.
PRIOR RECORDS:
- When starting case play, check for a prior chart or for additional patient information by clicking on the “EHR” button.
TAKING YOUR HISTORY:
- Step 1. Start by asking 2 open-ended patient centric questions:
- How can I help you today?
- Do you have any other symptoms or concerns we should discuss?
- Step 2. Obtain an HPI (History of Present Illness) using a mnemonic (OLDCARTS is one option):
When characterizing symptoms, ask questions based on building a differential or diagnosis for the patient.
Consider asking about the patient’s perspective:
- Tell me how that makes you feel.
- How does this affect your life?
- What symptom is the most distressing for you?
- Step 3. PMH (Past Medical History), FH (Family Health History), SH (Social History):
For patients with no prior chart, consider asking more past medical, social, and other questions than you might for a patient with a recent previous visit recorded.
For patients with a prior chart, still update allergies, medications, OTC drugs; update if major change in living situation, death of partner, loss of job, etc.
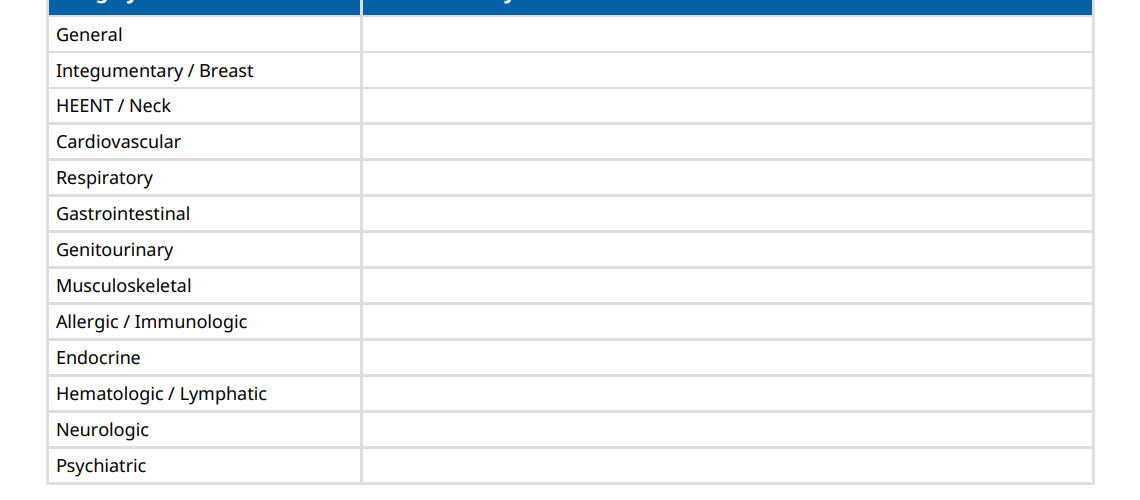
- Step 4. ROS (Review of Symptoms):
Questions for systems not addressed in HPI. Choose ROS for those body systems you do not have information on. Use the large multipart questions.
If you are not sure about the history questions to ask for any iHuman case, you can chat with one of our experts for Help.
HISTORY FEEDBACK TYPE:
- Your History Feedback is formatted to show the questions required by the case: what you asked and what was missed, organized according to the OLDCARTS mnemonic.
PHYSICAL EXAM:
- Notate your Key Findings in the “Key Findings” section, and document your Physical Exams in the EHR.
VITAL SIGNS – Optional
You must look at vitals in the EHR (Current Visit) to get credit.
PHYSICAL EXAM LIMIT:
- You can perform a limit of 40 exams.
- PERFORMING YOUR PHYSICAL EXAM:
- Always listen to the heart and lungs.
- Select other physical exams relative to your differential and/or the patient’s presented findings.
- To perform auscultation exams (heart, lung, etc):
- Select the exam
- Single click on the desired “hotspot” on the patient. Your cursor will turn into a stethoscope or gloved hand. A blue square will appear around the hotspot area indicating that the timer has begun
- Count using the timer above the patient’s head
- Repeat for other areas, then select interpretation
EXERCISES:
- Complete any clinical exercises found that follow various case play sections.
- When you’ve completed the exercises and clicked proceed, you will be taken to the next section.
- To skip over the exercises, click proceed to move forward with case play.
ASSESSMENT:
- Organize Key Findings: Record pivotal symptoms and signs that define and differentiate your top differential diagnoses.
PROBLEM STATEMENT:
- Short summary statement including: 1) relevant history findings first; 2) relevant physical examination findings; and 3) as many Key Findings as possible.
- Should be approx 150 words or less.
REVIEW TEST RESULTS:
- Review the test results (both images and interpretation) presented.
- Additionally, to review interim test results, review the Test Results tab in Prior Chart and/or the Patient Information tab in the Current Chart, if available.
SELECT DIAGNOSIS:
- Select a final diagnosis or diagnoses from the presented list.
PLAN:
- Write a medical note, SOAP note, management plan, or other document according to your instructor’s guidelines.
- Include pharmacologic therapies, supportive therapies, salient patient education, and instructions for follow-up including specific red flag symptoms that should prompt return.
- Consider the cost, risks, and benefits of various treatment plans.
- Please follow your instructor’s guidelines on what to include or what not to include in this section.
SUMMARY:
- Proceed all the way to the “Summary” tab.
- Submit your case, and press the “See Evaluation” button to view your performance evaluation, if available.